Orthopaedic Services
Get the orthopaedic care that you deserve.
Sports Medicine

Comprehensive Orthopaedic Care
We provide state-of-the-art digital radiology, ultrasound, physical therapy, and pain management services within our office. We also offer cortisone, platelet-rich plasma (PRP), and visco-supplementation injections, which promote tissue healing and are alternatives to surgery. Our focus is on treating every patient as an individual, not just an individual injury.
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
General
● Alternative Methods to Help Manage Pain After Orthopaedic Surgery
● Anesthesia for Hip and Knee Surgery
● Arthroscopy
● Articular Cartilage Restoration
● Bone Sarcoma in the Upper Extremity: Treatment Options Using Limb Salvage or Amputation
● Bone and Tissue Transplantation
● Bone, Joint, and Muscle Infections in Children
● Care of Casts and Splints
● Cortisone Injections
● Down Syndrome: Musculoskeletal Effects
● Exercise and Arthritis (video)
● Female Athlete Triad: Problems Caused by Extreme Exercise and Dieting
● Fractures (Broken Bones)
● Frequently Asked Questions About Stem Cells
● Frostbite
● Glucosamine and Chondroitin Sulfate
● Gout
● Growth Plate Fractures
● Heat Injury and Heat Exhaustion
● Helping Fractures Heal (Orthobiologics)
● Hemangioma
Shoulder & Elbow
● Arthritis of the Shoulder
● Biceps Tendinitis
● Biceps Tendon Tear at the Elbow
● Biceps Tendon Tear at the Shoulder
● Brachial Plexus Injuries
● Burners and Stingers
● Chronic Shoulder Instability
● Clavicle Fracture (Broken Collarbone)
● Common Shoulder Injuries
● Compartment Syndrome
● Dislocated Shoulder
● Distal Humerus Fractures of the Elbow
● Elbow (Olecranon) Bursitis
● Elbow (Olecranon) Fractures
● Elbow Arthroscopy
● Elbow Dislocation
● Elbow Fractures in Children
● Elbow Injuries in the Throwing Athlete
● Erb’s Palsy (Brachial Plexus Birth Palsy)
● Forearm Fractures in Children
● Frozen Shoulder
● Nursemaid’s Elbow
● Osteoarthritis of the Elbow
● Radial Head Fractures of the Elbow
● Recurrent and Chronic Elbow Instability
● Rotator Cuff Tears
● Rotator Cuff Tears: Frequently Asked Questions
● Rotator Cuff Tears: Surgical Treatment Options
● Rotator Cuff and Shoulder Conditioning Program
● SLAP Tears (labral Tears)
● Scapula (Shoulder Blade) Fractures
● Shoulder Arthroscopy
● Shoulder Impingement/Rotator Cuff Tendinitis
● Shoulder Injuries in the Throwing Athlete
● Shoulder Joint Tear (Glenoid Labrum Tear)
● Shoulder Pain and Common Shoulder Problems
● Shoulder Separation
● Shoulder Surgery
● Shoulder Surgery Exercise Guide
● Shoulder Trauma (Fractures and Dislocations)
● Tennis Elbow (Lateral Epicondylitis)
● Thoracic Outlet Syndrome
● Throwing Injuries in the Elbow in Children
● Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome)
Hand & Wrist
● Arthritis of the Hand
● Arthritis of the Thumb
● Arthritis of the Wrist
● Boutonnière Deformity
● Carpal Tunnel Syndrome
● Compartment Syndrome
● Complex Regional Pain Syndrome (Reflex Sympathetic Dystrophy)
● Congenital Hand Differences
● De Quervain’s Tendinosis
● Distal Radius Fractures (Broken Wrist)
● Dupuytren’s Contracture
● Finger Fractures
● Fingertip Injuries and Amputations
● Flexor Tendon Injuries
● Ganglion Cyst of the Wrist and Hand
● Hand Fractures
● Human Bites
● Lawn Mower Injuries in Children
● Mallet Finger (Baseball Finger)
● Nerve Injuries
● Scaphoid Fracture of the Wrist
● Sprained Thumb
● Thumb Fractures
● Trigger Finger
● Ulnar Tunnel Syndrome of the Wrist
● What is a Hand Surgeon?
● Wrist Arthroscopy
● Wrist Sprains
Hip & Thigh
● Adolescent Hip Dysplasia
● Burning Thigh Pain (Meralgia paresthetica)
● Deep Vein Thrombosis
● Developmental Dislocation (Dysplasia) of the Hip (DDH)
● Femoroacetabular Impingement
● Femur Shaft Fractures (Broken Thighbone)
● Hamstring Muscle Injuries
● Hip Bursitis
● Hip Conditioning Program
● Hip Dislocation
● Hip Fractures
● Hip Strains
● Inflammatory Arthritis of the Hip
● Intoeing
● Limb Length Discrepancy
● Muscle Strains in the Thigh
● Osteoarthritis of the Hip
● Pelvic Fractures
● Perthes Disease
● Preventing Blood Clots After Orthopaedic Surgery (video)
● Slipped Capital Femoral Epiphysis
● Snapping Hip
● Sports Hernia (Athletic Pubalgia)
● The Limping Child
● Thighbone (Femur) Fractures In Children
● Transient Osteoporosis of the Hip
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Foot & Ankle
● Adult Acquired Flatfoot
● Ankle Fractures in Children
● Anterior Cruciate Ligament (ACL) Injuries
● Arthritis of the Foot and Ankle
● Bunion Surgery
● Bunions
● Claw Toe
● Clubfoot
● Collateral Ligament Injuries
● Combined Knee Ligament Injuries
● Common Knee Injuries
● Corns
● Diabetic (Charcot) Foot
● Distal Femur (Thighbone) Fractures of the Knee
● Flexible Flatfoot in Children
● Foot and Ankle Conditioning Program
● Fractures of the Proximal Tibia (Shinbone)
● Growth Plate Fractures
● Hammer Toe
● Heel Pain
● Ingrown Toenail
● Intoeing
● Lawn Mower Injuries in Children
● Meniscus Tears
● Meniscus Tears (video)
● Morton’s Neuroma
● Orthotics
● Osgood-Schlatter Disease (Knee Pain)
● Plantar Fasciitis and Bone Spurs
● Posterior Tibial Tendon Dysfunction
● Rheumatoid Arthritis of the Foot and Ankle
● Sesamoiditis
● Shin Splints
● Stiff Big Toe (Hallux Rigidus)
● Stress Fractures
● Tarsal Coalition
● Vertical Talus
Neck & Back
● Back Pain in Children
● Cervical Fracture (Broken Neck)
● Cervical Radiculopathy (Pinched Nerve)
● Cervical Spondylosis (Arthritis of the Neck)
● Cervical Spondylotic Myelopathy (Spinal Cord Compression)
● Congenital Muscular Torticollis (Twisted Neck)
● Fracture of the Thoracic and Lumbar Spine
● Herniated Disk
● Herniated Disk in the Lower Back
● Idiopathic Scoliosis in Children and Adolescents
● Kyphosis (Roundback) of the Spine
● Low Back Pain
● Lumbar Spinal Stenosis
● Neck Pain
● Neck Sprain
● Osteoporosis and Spinal Fractures
● Sciatica
● Scoliosis: Frequently Asked Questions
● Spinal Deformity in Children with Myelomeningocele
● Spinal Injections
● Spine Conditioning Program
● Spondylolysis and Spondylolisthesis
Knee & Lower Leg
● Adolescent Anterior Knee Pain
● Arthritis of the Knee
● Bowed Legs (Blount’s Disease)
● Burning Thigh Pain (Meralgia paresthetica)
● Compartment Syndrome
● Deep Vein Thrombosis
● Discoid Meniscus
● Exertional Compartment Syndrome
● Intoeing
● Knee Arthroscopy
● Knee Arthroscopy Exercise Guide
● Knee Conditioning Program
● Knee Exercises
● Limb Length Discrepancy
● New Study Measures the Value of ACL Repair Surgery
● Osgood-Schlatter Disease (Knee Pain)
● Osteonecrosis of the Knee
● Osteotomy of the Knee
● Patellar Dislocation and Instability in Children (Unstable Kneecap)
● Patellofemoral Arthritis
● Pes Anserine (Knee Tendon) Bursitis
● Prepatellar (Kneecap) Bursitis
● Patellar (Kneecap) Fractures
● Patellar Tendon Tear
● Posterior Cruciate Ligament Injuries
● Quadriceps Tendon Tear
● Shin Splints
● Tibia (Shinbone) Shaft Fractures
● Preventing Blood Clots After Orthopaedic Surgery (video)
● The Limping Child
● Trauma Induced Compartment Syndrome
● Unstable Kneecap
● Viscosupplementation Treatment for Knee Arthritis
Osteoporosis
● Healthy Bones at Every Age
● Osteoporosis
● Osteoporosis Prevention
● Osteoporosis Prevention Starts Early
● Osteoporosis Tests
● Osteoporosis and Spinal Fractures
● Osteoporosis in Men
● Transient Osteoporosis of the Hip
● Weightbearing Exercise for Women and Girls

Sports Medicine
Together, our physicians and physical therapists have decades of cumulative experience treating athletes in every age group and at every level — whether they are competing in college athletics or simply want to stay fit and involved in the activities they enjoy.
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
General
● Female Athlete Triad: Problems Caused by Extreme Exercise and Dieting
● Heat Injury and Heat Exhaustion
● High School Sports Injuries
● Muscle Contusion (Bruise)
● Muscle Cramp
● Overuse Injuries in Children
● Skin Infections in Athletes
● Sports Concussion
● Sprains, Strains and Other Soft-Tissue Injuries
● X-rays, CT Scans and MRIs
Shoulder & Elbow
● Biceps Tendon Tear at the Shoulder
● Burners and Stingers
● Chronic Shoulder Instability
● Common Shoulder Injuries
● Dislocated Shoulder
● Elbow Injuries in the Throwing Athlete
● Rotator Cuff Tears
● SLAP Tears
● Shoulder Impingement/Rotator Cuff Tendinitis
● Shoulder Injuries in the Throwing Athlete
● Shoulder Joint Tear (Glenoid Labrum Tear)
● Shoulder Separation
● Tennis Elbow (Lateral Epicondylitis)
● Throwing Injuries in the Elbow in Children
Hand & Wrist
● Scaphoid Fracture of the Wrist
● Sprained Thumb
● Wrist Sprains
Hip & Thigh
● Hamstring Muscle Injuries
● Hip Bursitis
● Hip Strains
● Muscle Strains in the Thigh
● Snapping Hip
● Sports Hernia (Athletic Pubalgia)
Knee & Lower Leg
● Subchondroplasty
● Adolescent Anterior Knee Pain
● Anterior Cruciate Ligament (ACL) Injuries
● Collateral Ligament Injuries
● Combined Knee Ligament Injuries
● Common Knee Injuries
● Compartment Syndrome
● Meniscus Tears
● Meniscus Tears (video)
● Osgood-Schlatter Disease (Knee Pain)
● Patellar Dislocation and Instability in Children (Unstable Kneecap)
● Patellar Tendon Tear
● Patellofemoral Pain Syndrome
● Pes Anserine (Knee Tendon) Bursitis
● Posterior Cruciate Ligament Injuries
● Prepatellar (Kneecap) Bursitis
● Quadriceps Tendon Tear
● Shin Splints
● Stress Fractures
● Unstable Kneecap
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Foot & Ankle
● Ankle Fractures (Broken Ankle)
● Ankle Fractures in Children
● Lisfranc (Midfoot) Injury
● Sprained Ankle
● Stress Fractures of the Foot and Ankle
● Turf Toe
Neck & Back
● Low Back Pain
● Neck Pain
● Neck Sprain
Treatments & Surgeries
● Alternative Methods to Help Manage Pain After Orthopaedic Surgery
● Arthroscopy
● Articular Cartilage Restoration
● Cortisone Injections
● Elbow Arthroscopy
● Foot and Ankle Conditioning Program
● Hip Arthroscopy
● Hip Conditioning Program
● Knee Arthroscopy
● Knee Conditioning Program
● Managing Pain With Medications After Orthopaedic Surgery
● New Study Measures the Value of ACL Repair Surgery
● Orthotics
● Platelet-Rich Plasma (PRP)
● Rotator Cuff Tears: Surgical Treatment Options
● Rotator Cuff and Shoulder Conditioning Program
● Shoulder Arthroscopy
● Spine Conditioning Program
Injury Prevention
● Baseball Injury Prevention
● Basketball Injury Prevention
● Creatine Supplements
● Football Injury Prevention
● Golf Injury Prevention
● Gymnastics Injury Prevention
● Helmet Safety
● Hockey Injury Prevention
● Horseback Riding Injury Prevention
● Martial Arts Injury Prevention
● Return To Play
● Safe Exercise
● Shoes: Finding the Right Fit
● Skiing Injury Prevention
● Soccer Injury Prevention
● Sports Injury Prevention for Baby Boomers
● Sports Nutrition
● Swimming Injury Prevention
● Tennis Court Safety
● Tennis Injury Prevention
● The Risks of Steroid Use
● Tips for a Safe Running Program
● Train Smart and Stay Strong
● Trampoline Injury Prevention
● Volleyball Injury Prevention
● Winter Sports Injury Prevention
● Yoga Injury Prevention
Health & Fitness
● Aerobic Exercise
● Athletic Shoes
● Bicycle Safety
● Creatine Supplements
● Cross Training
● Distracted Walking
● Diving Safety
● Effects of Aging
● Exercise Walking
● Exercise and Bone Health
● Exercise and Bone and Joint Conditions
● Female Athlete Triad: Problems Caused by Extreme Exercise and Dieting
● Fitness for Kids
● Flexibility Exercises for Young Athletes
● Healthy Bones at Every Age
● Helmet Safety
● Osteoporosis Prevention Starts Early
● Physical Activity for Persons with Mental Retardation
● Rehabilitation Exercise and Conditioning Handouts
● Safe Exercise
● Selecting Home Exercise Equipment
● Seniors and Exercise
● Seniors and Exercise: Starting an Exercise Program
● Sports Injury Prevention for Baby Boomers
● Sports Nutrition
● Starting a Strength Training Program
● Starting an Exercise Program
● Staying Active As You Age
● The Impact of Childhood Obesity on Bone, Joint, and Muscle Health
● The Risks of Steroid Use
● Tips for a Safe Running Program
● Train Smart and Stay Strong
● Vitamin D for Good Bone Health
● Warm Up, Cool Down and Be Flexible
● Weightbearing Exercise for Women and Girls
● Why Exercise?

Joint Replacement
Leading the way, we started the outpatient joint replacement center at Danbury Hospital; we help our patients decide if this progressive approach meets their individual needs. According to recent data, we have exceptionally low complication rates that are well below national standards and unequaled in the area.
Nuvance Health Surgical Patients
Our Nuvance Health surgical patients can access detailed information on our knee and hip replacement procedures and what to expect by reviewing our guidebooks:
● Download Knee Replacement Guide
● Download Hip Replacement Guide
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Diseases & Conditions
● Arthritis of the Knee
● Arthritis of the Shoulder
● Arthritis of the Thumb
● Arthritis of the Wrist
● Arthritis: An Overview
● Cervical Spondylosis (Arthritis of the Neck)
● Gout
● Inflammatory Arthritis of the Hip
● Juvenile Arthritis
● Osteoarthritis
● Osteoarthritis of the Elbow
● Osteoarthritis of the Hip
● Osteonecrosis of the Hip
● Patellofemoral Arthritis
● Rheumatoid Arthritis
● Rheumatoid Arthritis of the Foot and Ankle
● Synovial Chondromatosis
Treatments & Surgeries For Arthritis
● Articular Cartilage Restoration
● Elbow Arthroscopy
● Exercise and Arthritis (video)
● Exercise and Bone and Joint Conditions
● Glucosamine and Chondroitin Sulfate
● How to Use Crutches, Canes and Walkers
● Knee Arthroscopy
● Knee Arthroscopy Exercise Guide
● Makoplasty of the Hip
● Makoplasty of the Knee
● Managing Arthritis Pain With Exercise
● Spinal Injections
● Stem Cells and Orthopaedics
● Subchondroplasty of the Knee
● Total Hip Replacement Module
● Total Knee Replacement Module
● Viscosupplementation Treatment for Knee Arthritis
● What Are NSAIDs?
General
● Anesthesia for Hip and Knee Surgery
● Before and After Total Joint Replacement (video)
● Cortisone Injections
● Managing Pain With Medications After Orthopaedic Surgery
● Obesity, Weight Loss, and Joint Replacement Surgery
● Platelet-Rich Plasma (PRP)
● Preparing for Joint Replacement Surgery
● Preventing Blood Clots After Orthopaedic Surgery (video)
● Preventing Infection After Joint Replacement Surgery (video)
● Total Joint Replacement
● Total Joint Replacement: Questions Patients Should Ask Their Surgeon
Shoulder
● Shoulder Joint Replacement
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Hand & Wrist
Hip & Thigh
● Dislocation After Total Hip Replacement (video)
● Fracture After Total Hip Replacement
● Hip Resurfacing
● Minimally Invasive Total Hip Replacement
● Makoplasty of the Hip
● Preventing Blood Clots After Orthopaedic Surgery (video)
● Total Hip Replacement
● Total Hip Replacement Exercise Guide
Knee & Lower Leg
● Knee Replacement Implants
● Subchondroplasty of the Knee
● Makoplasty of the Knee
● Minimally Invasive Total Knee Replacement
● New Study Finds that Knee Replacement Is A Cost-Effective Treatment Option
● Preventing Blood Clots After Orthopaedic Surgery (video)
● Revision Total Knee Replacement
● Total Knee Replacement
● Total Knee Replacement Exercise Guide
● Unicompartmental Knee Replacement
Considerations
● Fracture After Total Hip Replacement
● Joint Replacement Infection

Pain Management
We also have expertise in regenerative medicine techniques, including stem cell therapy (SCT) and platelet-rich plasma (PRP) injections. These leading-edge technologies involve injecting damaged tissue with a patient’s own stem cells or plasma. While the new cells adapt to their environment, they repair damage in the process. Many of these techniques offer relief for patients with chronic pain who have not responded to traditional treatment. Our goal is to return our patients to their everyday activities quickly, decrease their need for medication, and improve their overall quality of life.
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Conditions
● Arthritis (Knee/Hip, etc)
● Back Pain
● Bone Spurs/Osteophytes
● Complex Regional Pain Syndrome (CRPS)
● Degenerative Disc Disease
● Facet Joint Syndrome
● Failed Back Surgery Syndrome
● Headaches
● Herniated/Bulging Disc
● Neck Pain
● Neuropathy
● Pinched Nerve
● Radiculopathy
● Sacroiliac (SI) Joint Pain
● Sciatica
● Spinal Stenosis
● Spine Compression Fractures
● Spondylosis/Spine Arthritis
Treatments
● Discography
● Epidural Steroid Injections
● Facet Joint Injection
● Intradiscal Therapy / Biacuplasty
● Intrathecal Drug Delivery (IT-Pump)
● Kyphoplasty/Vertebroplasty
● Lumbar Sympathetic Block
● Platelet-Rich Plasma (PRP)
● Nerve Root Block
● Non-Surgical Treatment for Disc Herniation (Percutaneous Discectomy)
● Radiofrequency Ablation
● Radiofrequency Neurotomy
● Regenerative Medicine: Stem Cell Autologous Transplantation
● Shoulder, Hip, and Knee Joints Injection
● Spinal Cord Stimulator
● Stellate Ganglion Block

Radiology & Digital X-Rays
We also use a highly sophisticated fluoroscopic and mobile imaging unit for X-Ray localization during interventional pain management procedures.
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Imaging studies performed somewhere else
Pickup your X-Rays

MAKOplasty Robotic Arm Partial Knee Resurfacing
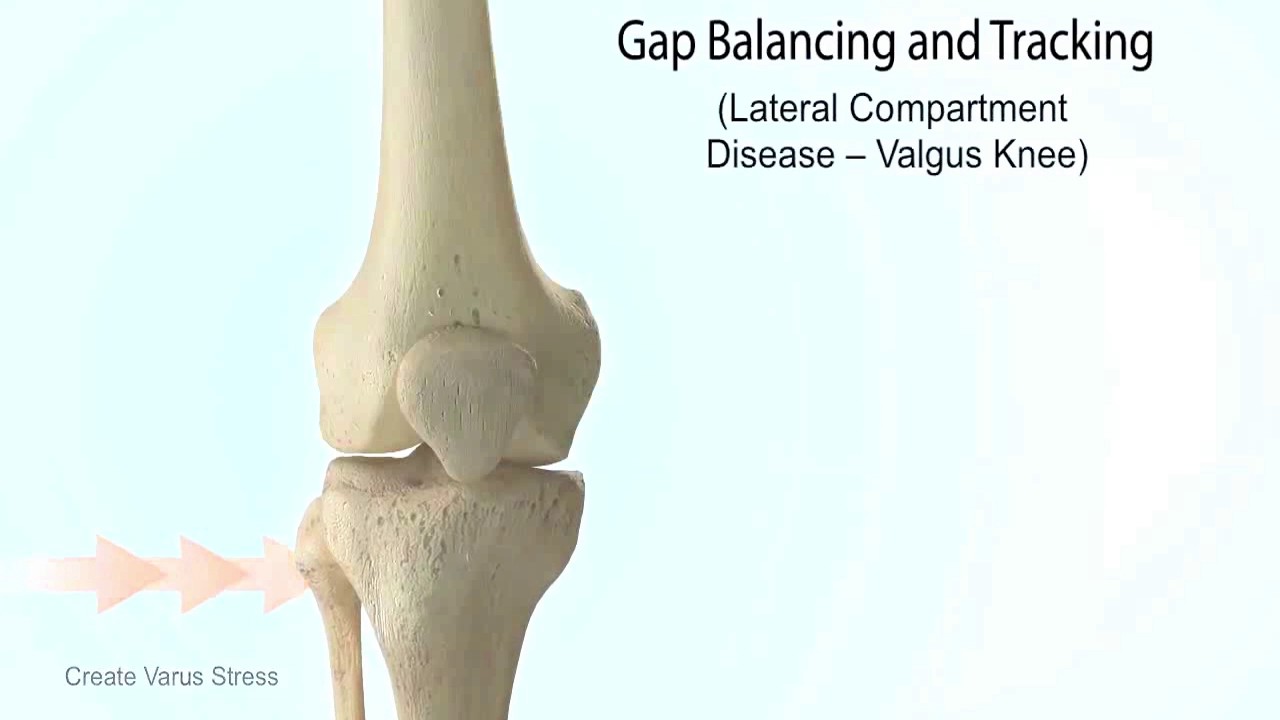
MAKOplasty is designed to relieve the pain caused by joint degeneration due to osteoarthritis (OA). By selectively targeting only the diseased part of your knee, your surgeon can spare healthy bone, tissue, and ligaments. Other benefits may include a smaller incision, shorter hospital stay, less pain, reduced blood loss, less scarring, and a more rapid recovery.
MAKOplasty is indicated for patients suffering from osteoarthritis in one or two compartments of their knee. A total knee replacement is sometimes necessary if your surgeon discovers during surgery that your knee has more damage than originally seen in the pre-operative X-rays and CT scan.
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
MAKOplasty – A Less Invasive Procedure
By preserving healthy bone, tissue, and ligaments, along with more accurate implant positioning, you can expect a more natural feeling knee. Since healthy bone is preserved, patients who undergo MAKOplasty partial knee procedures may still be candidates for a total knee replacement procedure later in life if necessary. Your surgeon should discuss the specific risks associated with MAKOplasty and other treatment options with you.
Clinical Data Highlights
Comparing American Knee Society Scores, a common measure of knee functionality, the study also found MAKOplasty patients had increased post-operative functionality at three months post-surgery.
Is MAKOplasty® covered by health insurance providers?
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
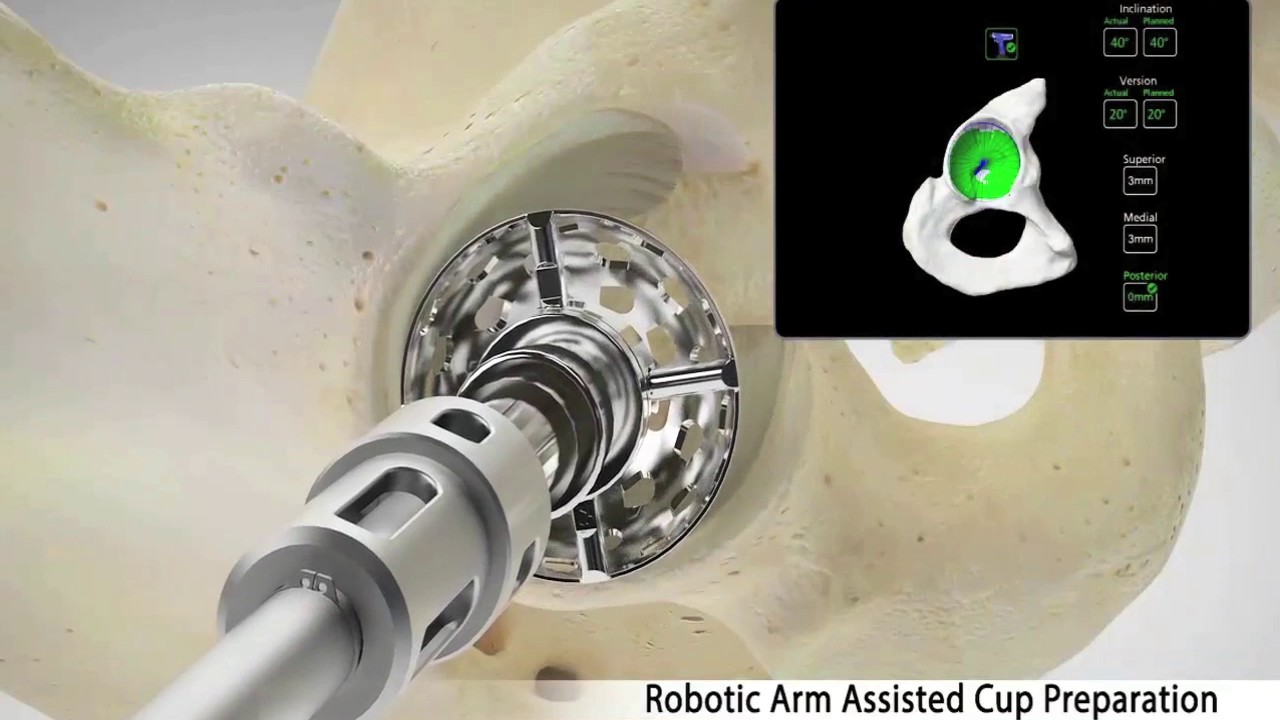
Does the robotic arm system actually perform the surgery?
The robotic arm does not perform the surgery, nor can it make decisions on its own or move in any way without the surgeon guiding it. During surgery, RIO® provides the surgeon with real-time visual, tactile, and auditory feedback to facilitate optimal joint resurfacing and implant positioning. It is this optimal placement that can result in more natural knee motion following surgery.
What is the difference between MAKOplasty and traditional knee replacement surgery?
What is the lifespan of a MAKOplasty implant?

MAKOplasty Robotic Arm Total Hip Arthroplasty
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Understanding Degenerative Joint Disease
Degenerative joint disease (DJD) can cause a loss of cartilage, resulting in bone-on-bone contact that may result in pain, swelling, and stiffness. There are different types of DJD that may cause hip pain.
What is degenerative joint disease (DJD) of the hip?
● Osteoarthritis (OA): also called “wear-and-tear arthritis,” in which the cartilage wears down over time.
● Post-traumatic arthritis: which results from a severe fracture or dislocation of the hip.
● Rheumatoid arthritis (RA): an inflammatory arthritis of the joints.
● Avascular necrosis (AVN): a condition where the “ball” or femoral head has lost a healthy supply of blood flow, causing the bone to die and the femoral head to become misshapen.
● Hip dysplasia: a developmental deformation or misalignment of the hip joint.
If you are one of the millions of Americans suffering with hip pain from degenerative joint disease, you may be a candidate for MAKOplasty® total hip arthroplasty, also known as MAKOplasty® total hip replacement.
What is MAKOplasty Total Hip Replacement?
Display: none
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
How does MAKOplasty® work?
What are the potential benefits of MAKOplasty® robotic arm-assisted hip replacement?
The RIO® System software uses patient-specific anatomic information from a pre-operative CT scan to enable the accurate position of the implants so that the likelihood of implant or bony impingement is reduced as well as a possible reduction in the rate of dislocation.
The RIO® System allows the surgeon to know and control the position of the cup and stem in addition to the final correction of leg length accomplished by the hip replacement before closing the incision.
Who is a good candidate for the MAKOplasty® total hip procedure?
● Pain while putting weight on the affected joints.
● Limping to lessen the weight-bearing pressure on the hip.
● Hip pain or stiffness during walking or other impact activities.
● Failure to respond to non-surgical treatments or pain medication.
● Be sure to discuss all treatment options with your doctor.
Treat you injuries with Orthopaedic Specialists of Connecticut.
Why Choose Us
Personal Care
Teamwork
Surgical Outcomes
All Rights Reserved Orthopaedic Specialists of Connecticut